Meningioma tumors
Overview
A meningioma is a tumor that grows from the membranes covering the brain and spinal cord. Most meningiomas are benign (not cancer) and slow growing. Yet, some can be aggressive (malignant). Symptoms often appear gradually and vary depending on the tumor location. Because of their slow growth, not all meningiomas need treatment right away. They can be watched over time. If the tumor grows or symptoms worsen, then surgery or radiation are options.
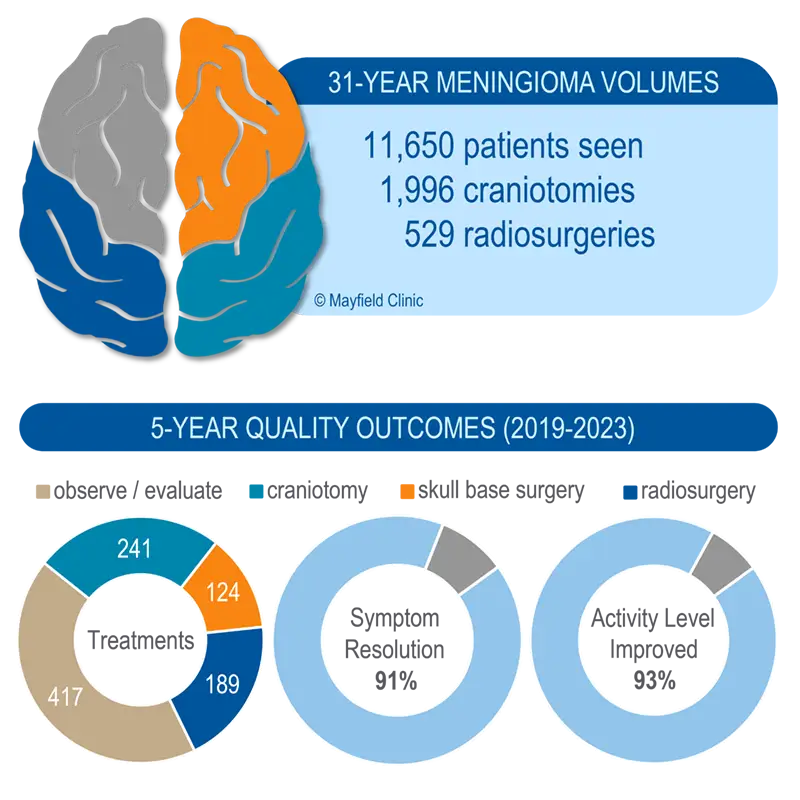
In the past 5 years, Mayfield has seen 2,971 patients with meningiomas and performed 542 procedures — making Mayfield a high-volume treatment program.1 In context, nearly a quarter of people newly diagnosed with a meningioma in Ohio2 seek care at Mayfield, many of which are observed.
We are affiliated with premier hospital systems in the Cincinnati, Dayton and Northern Kentucky regions. Treatment options include skull base surgery, minimally invasive keyhole and endoscopic surgery, Gamma Knife radiosurgery, radiotherapy, and careful observation.
Mayfield is a member of the NeuroPoint QOD Tumor Registry that collects outcomes data to improve quality of care for all brain tumor patients. See our meningioma volumes, quality of care, and publications.
To make an appointment call 513-221-1100.
What is a meningioma?
Meninges are three membranes that line the skull and spinal canal, protecting the brain and spinal cord. From the outermost layer inward they are: the dura, arachnoid, and pia. A meningioma tumor grows from the arachnoid cells attached to the dura (Fig. 1). Meningiomas tend to grow inward. Their mass pushes on the brain, nerves, and blood vessels. They can also grow outward, causing the skull to thicken (hyperostosis). Some contain fluid cysts or calcified deposits. Others contain many tiny blood vessels. Multiple meningiomas are seen in 10% of patients.

What are the symptoms?
Meningiomas grow slowly and may not cause symptoms for years. Some people with have no symptoms. A tumor may be found incidentally on an MRI or CT scan done for another reason. If patients have symptoms, they can vary by the location and size of the tumor. They often first appear as headaches or seizures, caused by pressure on the brain. Dizziness, weakness in the arms or legs, vision changes, may occur with meningiomas.
Meningiomas are named according to their location (Fig. 1) and cause various symptoms:
- Convexity meningiomas: grow on the surface of the brain. They may not produce symptoms until they reach a large size. Symptoms may include seizures, neurological deficits, or headaches.
- Falx and parasagittal meningiomas: grow from the dura between the left and right sides of the brain. The falx contains two large blood vessels (sinuses) that can make removal more difficult. Symptoms may include personality changes, headache, vision problems, and weakness.
- Olfactory groove meningiomas: grow along the nerves to the nose and cause a loss of smell. Compression of the frontal lobes causes personality changes, which may be mistaken for depression. They can compress the optic nerves, causing visual problems.
- Tuberculum sella meningiomas: grow near the pituitary gland and optic nerves. They often cause visual field problems.
- Sphenoid meningiomas: grow along the skull base behind the eyes. These tumors can cause visual problems, bulging of the eye, or facial numbness. They often encase the cavernous sinus, carotid arteries, and cranial nerves. This makes them difficult to completely remove.
- Posterior fossa meningiomas: grow along the skull base near the brainstem and cerebellum. They compress the cranial nerves, causing facial symptoms, hearing loss, a hoarse voice, or swallowing problems. Petroclival tumors can compress the trigeminal nerve, resulting in facial pain or numbness.
- Foramen magnum meningiomas: grow where the spinal cord connects to the brain. They can cause headaches, brainstem compression, and difficulty walking.
- Intraventricular meningiomas: grow inside the fluid-filled ventricles of the brain. They block the flow of CSF fluid causing hydrocephalus, headaches, memory issues, and difficulty walking.
- Intraorbital meningiomas: grow around the eye sockets and push on the eyes. This gives the eyes a bulging appearance (proptosis) and can cause loss of vision.
- Spinal meningiomas: grow mainly in the thoracic spine and cause back pain (typically at night). They compress the spinal cord and can cause loss of sensation or paralysis of the legs.
What are the causes?
Scientists are not certain what causes brain tumors, but there are known risk factors. An alteration in chromosome 22 is the most common abnormality in meningiomas.
- Neurofibromatosis type 2 (NF2). People with NF2 are more likely to develop meningiomas.
- Radiation exposure. Radiotherapy to the head for other conditions increases risk for meningiomas later in life.
- Female hormones. About 70% of meningiomas have progesterone receptors, and 10% have estrogen receptors. This may explain why meningiomas tend to grow during pregnancy.
Patient Stories
Who is affected?
Meningiomas account for 37% of all primary brain tumors and 12% of all spinal cord tumors. They are often found in adults and the risk increases with age over 65 years. Most are benign (not cancer) and are three times more common in women.
How is a diagnosis made?
The doctor will ask about your medical history and perform a neurological exam. Some of the tests may check your mental status and memory, cranial nerve function, muscle strength, coordination, reflexes, and response to pain.
Computerized tomography (CT) or magnetic resonance imaging (MRI) scans are done to evaluate the size, location, and mass effect of the tumor (Fig. 2). Other tests may include angiograms of the blood vessels, visual field acuity test, or hearing test.


What treatments are available?
A treatment plan is personalized for you. It may involve a combination of therapies. Factors include your age, general health, and the tumor location, size, and grade. Each treatment has benefits, risks, and side effects that should be discussed and understood.
Observation ("watch and wait")
Because meningiomas grow slowly, small or medium size tumor with no or few symptoms may be observed. The doctor will monitor the tumor’s growth with periodic MRI scans. The tumor volume is compared to previous scans to calculate a growth rate. Patients should immediately report any change in their symptoms. If the tumor grows, surgical removal or stereotactic radiosurgery are options.
Surgery
If a meningioma is large, causing symptoms, or is growing, surgical removal is often recommended. A craniotomy surgery opens the skull to remove the tumor (Fig. 3). Although total removal can provide a cure for meningioma, it is not always possible. The tumor location determines how much can be safely removed. If some tumor is left attached to arteries or nerves, radiation can treat the remainder. The risks of surgery depend on where the tumor is located.

Technologies improve the surgeon’s ability to locate the tumor and avoid injury to vital brain areas. These include:
- Brain mapping functional MRI (fMRI) detects blood oxygen levels in brain areas responsible for movement, speech, and perception. By “mapping” these eloquent areas, surgeons can remove tumors without harming areas that are critical to the patient’s quality of life.
- Tumor embolization is a biologic glue used to block the blood vessels feeding the tumor, making it easier to remove. It also reduces bleeding during surgery. The glue is delivered through a catheter during an angiogram.
- Image-guided surgery (IGS) helps the surgeon pinpoint the exact location of a tumor. An MRI scan with markers placed on the patient’s head is taken before surgery. During surgery, the markers correlate the “real patient” lying on the table to a 3D model of their MRI scans. IGS allows precise pinpointing of the tumor edges, guides the skin and bone openings, and tracks tumor removal (Fig. 4).
- Keyhole & endoscopic surgery are minimally invasive techniques. Surgeons remove tumors at the skull base through small keyhole openings, such as through the nose, eyelid, or eyebrow. By operating through a natural pathway, surgery can be performed without a visible scar on the face or scalp.

Tumor cell analysis and biomarkers
During surgery, samples of tumor cells are taken (biopsy). These are examined under a microscope by a pathologist to confirm the tumor type and grade. There are 3 grades of meningiomas:
- Grade I, benign meningiomas are the slowest growing. About 80% of tumors are grade 1. Patients who undergo complete removal of a grade I meningioma usually require only surveillance MRI scans. Patients who undergo incomplete removal may need radiation after surgery.
- Grade II, atypical meningiomas grow more aggressively and have a higher risk of recurrence. Surgery is the first line of treatment. Some will require radiation after surgery. About 18% of tumors are grade 2.
- Grade III, anaplastic meningiomas are the most aggressive and often recur. For malignant meningiomas, surgery is the first line of treatment, followed by radiation. If the tumor recurs, chemotherapy is used. About 2% of tumors are grade 3.
Two additional tests are routinely performed on the biopsy sample. The proliferative index measures the percent of tumor cells that are actively dividing and growing. Molecular profiling reveals DNA mutations that can help predict how a tumor will behave and respond to treatment.
Radiation
Indications for radiation include: (1) small to medium-size tumors without symptoms, (2) incomplete tumor removal, (3) inoperable tumors, (4) malignant meningioma, and (5) patient choice. Radiation damages the DNA inside the cells, making them unable to divide and reproduce. The goal is to maximize the dose to abnormal tumor cells and minimize exposure to normal healthy cells (Fig 5). The benefits of radiation are not immediate but occur over time. Gradually, the tumor stops growing and occassionally can shrink. Benign tumors, whose cells divide slowly, may take several years to show an effect. Radiation therapy options for meningiomas include:
- Stereotactic radiosurgery delivers a high dose of radiation during a single session or 5 daily sessions. Although it is called surgery, no incision is made. Because the radiosurgery dose is high, the target area must be completely immobilized with a stereotactic head frame or facemask. Patients spend most of the day at the center while the tumor is precisely located, a treatment plan is developed, and a radiation dose is delivered.
- Fractionated radiotherapy delivers lower doses of radiation over several weeks. A facemask is used to accurately reposition the patient for each treatment session. Delivering a fraction of the total radiation dose each day allows normal cells time to repair themselves between treatments. It also reduces side effects. Patients return 5 days a week for 5 to 6 weeks to receive the complete radiation dose.
- Proton beam therapy delivers accelerated proton energy to the tumor at a specific depth. The radiation beam does not go beyond the tumor.

Figure 5. A radiosurgery treatment plan for a meningioma in the cavernous sinus. The rings represent the radiation dose delivered to the tumor. 
Figure 6. Radiation is delivered by a machine that rotates around the patient, aiming beams that are shaped to match the tumor and minimize exposure to normal brain tissue.
Chemotherapy and biologics
Chemotherapy is rarely used. It is an option reserved for malignant or recurrent meningiomas. Medical therapies may include:
- Hydroxyurea is a chemotherapy pill that inhibits tumor cell DNA replication.
- Alpha interferon is a biologic therapy injection that inhibits tumor blood vessel growth.
- Sandostatin is a hormone therapy injection that suppresses tumor growth. A nuclear imaging study is first performed to determine if the tumor has somatostatin receptors.
- Avastin is a biologic therapy injection that inhibits tumor blood vessels and starves the tumor.
Clinical trials
Clinical trials are research studies in which new treatments – drugs, diagnostics, procedures, vaccines, and other therapies – are tested in people to see if they are safe and effective. Research is always being conducted to improve the standard of medical care. Information about current clinical trials is online at ClinicalTrials.gov and CenterWatch.com.
Recovery
The location and grade of the tumor are the most important factors in your outcome and prognosis. Convexity, parasagittal, and sphenoid wing meningiomas usually are completely removable, and surgery can yield excellent results. Optic, cavernous sinus, and skull base meningiomas have a higher rate of complication and are more difficult to completely remove. The patient's age and overall health prior to surgery may also affect the results. Some meningiomas do recur after surgery or radiation. Regular follow-up MRI or CT scans (1 to 2 years) are an important part of long-term care for anyone diagnosed with a meningioma.
Sources & links
If you have more questions, please contact Mayfield Brain & Spine at 800-325-7787 or 513-221-1100.
Support
Support groups provides an opportunity for patients and their families to share experiences, receive support, and learn about advances in treatments and medications.
Links
American Brain Tumor Association (ABTA.org)
1.800.886.2282
National Brain Tumor Society (braintumor.org) at 1-800-934-2873
Glossary
anaplastic: when cells divide rapidly and bear little or no resemblance to normal cells in appearance or function.
benign: does not invade nearby tissues or spread; not cancerous.
biopsy: a sample of tissue cells for examination under a microscope to determine the existence or cause of a disease.
edema: tissue swelling caused by the accumulation of fluid.
hyperostosis: an excessive growth of bone.
meninges: three membranes (pia mater, arachnoid mater, and dura mater) that surround the brain and spinal cord.
hemangiopericytoma: very uncommon type of meningioma, highly vascular and usually fast growing.
mass effect: damage to the brain due to the bulk of a tumor, the blockage of fluid, and/or excess accumulation of fluid within the skull.
malignant: having the properties of invasive growth and ability to spread to other areas; cancerous.
meningioma: a tumor that grows from the meninges, the membrane that surrounds the brain and spinal cord.
updated > 12.2024
reviewed by > Ronald Warnick, MD, Yair Gozal, MD, PhD, Mayfield Clinic, Cincinnati, Ohio
 Mayfield Certified Health Info materials are written and developed by the Mayfield Clinic. This information is not intended to replace the medical advice of your health care provider.
Mayfield Certified Health Info materials are written and developed by the Mayfield Clinic. This information is not intended to replace the medical advice of your health care provider.

 Brooke's story > Skull base meningioma
Brooke's story > Skull base meningioma Patrick's story > Parafalcine meningioma
Patrick's story > Parafalcine meningioma Vivien & Ruth's story > multiple meningiomas
Vivien & Ruth's story > multiple meningiomas