
Terry’s story
Scoliosis, decompression and fusion surgery
Spinal deformity surgery helps Terry get "better and better"
"I was getting worse and worse," Terry says, "and now I'm getting better and better."
For several years, intense back pain had spread down her left leg and produced stabbing pain across to her right side. She says she always felt "weighed down."
That led to bookend surgeries that made 2023 quite an eventful year for Terry. In January, she underwent a hip replacement. That had not relieved all of her symptoms, and scans showed a side-to-side curvature of her spine, called scoliosis.
On the day after Christmas, she went into the hospital for a two-phase surgery to stabilize and rebuild the lower portion of her spine. After the spine operation with Dr. Brad Curt of Mayfield Brain & Spine, she still felt some surgical pain. But the numbness, weakness and shooting pain were gone.
Dr. Curt says Terry's spine was degenerating at multiple levels, and the natural history of the disease was likely to require a total reconstruction from the level of her ribcage all the way down to her pelvis.
"The severe stenosis, or narrowing of the spinal canal, was just one of the conditions that were causing Terry's pain," Dr. Curt says. "Several of the vertebrae in her lumbar spine had slipped out of alignment. But the unnatural curvature was clearly reflected in her imaging, and we recommended a global solution that would realign and strengthen the entire lower portion of her spine."

Terry pushed off the surgery while she tried more conservative measures, such as physical therapy and pain injections. Several months later, as the symptoms worsened and the scans showed continued deterioration, she decided to proceed with the operation.
"I was stressed out about that, because I could see it as it was happening," she says.
Today, Terry is back to biking, hiking and more of her favorite outdoor activities, "doing things now that I haven't been able to do in years."
Back pain had been building
Terry's pain started nearly a decade ago, mostly in her hip and eventually migrating to her lower back. It mostly bothered her during periods of activity. She tried to manage the pain as much as she could.
"All that kind of stooping and twisting, it really bothered me," she recalls now. "I was just being stabbed and poked all day long. It was kind of exhausting."
Terry works in the operating room at a local hospital. She consulted with Mayfield and decided to proceed cautiously. Since she was training for a half-marathon with her husband and son, she wanted to avoid surgery if possible.
But that changed in 2021, when the numbness and weakness started creeping down her left leg. Her biggest problem then was her hip, and she took injections to ease that pain as well.
"At that point, I almost couldn't walk," she says.
She proceeded with the hip replacement. But even after that operation, Terry still felt pain in her lower back and down her leg, and crossing into her right buttock. She consulted with Dr. Curt, part of Mayfield's Scoliosis and Spinal Deformity team, eventually deciding to proceed with the surgery.
For major spinal deformity cases like Terry's, the surgery goes in two phases. First, Dr. Curt performed an anterior lateral interbody fusion, known as ALIF, to repair damage from the L3-S1 levels of her spine. After a three-day period to monitor her progress and ensure she was prepared for additional surgery, Terry returned to the operating room for phase two. Dr. Curt and fellow neurosurgeon Dr. Randy Hlubek relieved the pressure on nearby nerves through decompression, then fused the entire spine together, starting from the T10 vertebrae in the middle of her back all the way through the base of her spine to the pelvis.
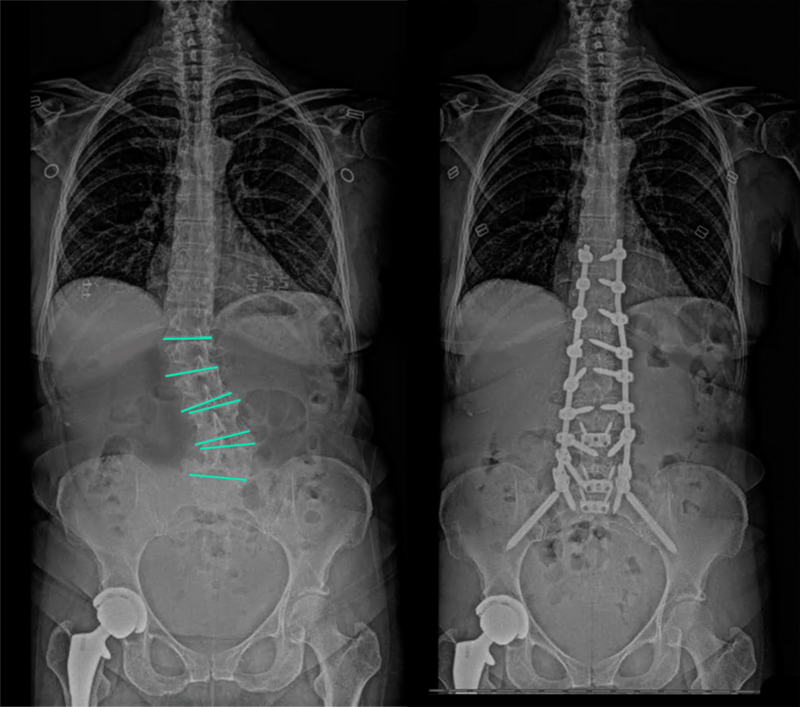
"Our first job was to repair Terry's lumbar spine that was being hampered by severe stenosis and related spondylolisthesis," Dr. Curt says. "In the second phase of the surgery, we corrected the scoliosis and restored a natural curvature to her spine up to the T10 level, then stabilized the spine with internal hardware to allow it to heal in the proper position."
The complex two-stage surgery can lead to recovery time of six months or even longer. Patients undergo a series of diagnostic tests before they reach the operating room. They also must take steps to promote bone growth – including stopping smoking or tobacco use.
"Spinal deformity surgery has the potential to really enhance the lives of patients by restoring their ability to be active and do the things they love to do," Dr. Curt says. "Terry is realizing those benefits now, and she should continue to improve as her spine heals and grows stronger."
Seven days after checking into the hospital, Terry went home. She worked from home for several months, but recently has resumed her job in a local hospital. She recognizes the difficulty of such a major surgery – but she's glad she made that choice.
"On the one hand, it's not something I would recommend lightly," she says. "On the other hand, if you need it, it sure can make a difference in your life."
~ Cliff Peale
Hope Story Disclaimer -"Terry's Story" is about one patient's health-care experience. Please bear in mind that because every patient is unique, individual patients may respond to treatment in different ways. Results are influenced by many factors and may vary from patient to patient.
