
Sara's story
Pelvic floor dysfunction
Specialized physical therapy helps Sara reduce effects of pelvic floor dysfunction
The difficulty started, Sara remembers, with pain and stiffness in her core. She suffered some sharp pain in her abdomen after her third C-section. Sleeping through the night and emptying her bladder became issues. Her hips sometimes locked up getting up off the floor while playing with her kids.
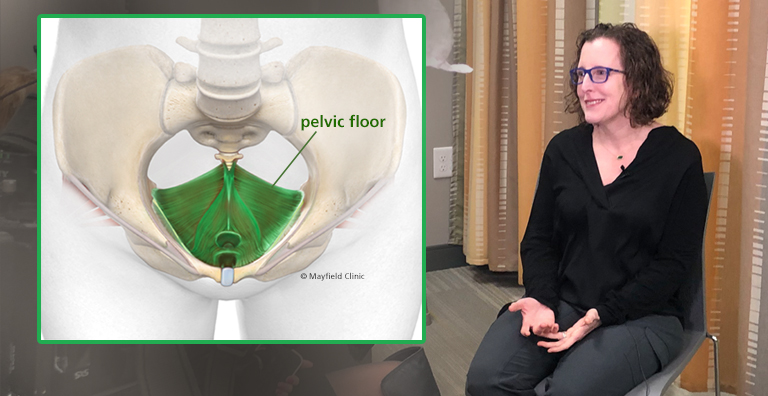
After consultations with her physician, she was referred to Mayfield and to Lisa Johnstone, a physical therapist specializing in pelvic floor dysfunction – when the muscles that line the bottom of the pelvis are too tight or too weak. The effects can be widespread, from bowel and bladder issues to pelvic pain or post-pregnancy pain.
"I was super-tight. All of the muscles were tight," Sara says. "Working with Lisa just helped loosen up those muscles and gain strength in the right places."
More than 25 percent of women and up to 10 percent of men can suffer the symptoms of pelvic floor dysfunction, Johnstone says. Diagnosed or referred by urologists or other specialists, patients often use specialized physical therapy as a first step in their treatment plan.
First, the physical therapist will conduct an assessment and go through a series of traditional PT exercises to test strength and range of motion for the hips, lower back and core area. Second, the therapist will conduct an examination in a private room, testing the pelvic muscle manually. It can seem like an OB/Gyn visit for women or a prostate exam for men.
"Like any muscle, the pelvic floor can be injured or become weakened over time," Johnstone says. "Also like any muscles, the pelvic floor can gain strength and become more flexible and functional. We design a custom treatment plan for each patient, based on the symptoms they are experiencing and the goals they are trying to achieve."
Read Lisa Johnstone's Q&A on pelvic floor dysfunction
For Sara, those goals were simple: reducing the pain that followed her last childbirth and gaining strength and mobility in her hips and lower back. She says the physical therapy sessions with Johnstone cleared up some of her misconceptions about pelvic floor treatments.
"It was not as invasive as I thought it would be," Sara says. "Even being able to sit up more easily, it helps in so many different areas. My ability to sleep through the night and empty my bladder – I didn't know that was a problem I could fix with physical therapy."
Sara recalls that after an earlier knee surgery, she was in physical therapy within a few days. But after three invasive C-section surgeries, she got no extra treatment at all. Specialized pelvic floor treatments fill the gap, she says. Now, she does a full range of exercises at home and gets some dry needling from Johnstone to help stimulate healing.
"I've got a lot of scar tissue," she says. "Dry needling helps to break up the scar tissue. I just don't want any of these symptoms to slip backwards."
~ Cliff Peale
Hope Story Disclaimer -"Sara's Story" is about one patient's health-care experience. Please bear in mind that because every patient is unique, individual patients may respond to treatment in different ways. Results are influenced by many factors and may vary from patient to patient.

