
Lisa's story
Severe scoliosis
Lisa thought long and hard about whether to undergo major spine surgery for severe scoliosis. The abnormal curvature of her spine had been with her since childhood, but it was worse now that she was in her early 50s. She also suffered from rheumatoid arthritis, and she had been seeing a pain management specialist for more than a decade. She was able to work, but her life was becoming more and more difficult.
"I couldn't participate in things everyone else was doing," she says. "I was always looking for something to lean on, or someplace to sit. I just could not keep up. And even if I could, I was always hot and sweaty because I was in overdrive. I didn't think I could participate fully in things we were doing as a family or even with friends. I wouldn't say I missed out, but I struggled."
Still, she thought long and hard, not only about having complex spinal surgery, but also about the recovery, which would take months. Surgeons measure the outcome for major spinal deformity surgery at one year.
"I work full-time; I live alone," she muses. "I do laundry, the housekeeping. I have a dog. All of those things I had to think about because I was going to be on my own afterward. On the flip side, I was going to have to grow old doing those things by myself with my health just getting worse."
As the compression, stenosis, and deterioration in her spine gradually built, and as her need for medications became unmanageable, Lisa made her decision to forge ahead. Her pain management specialist, Tammy Musolino, MD, of TriHealth, referred her to Michael Kachmann, MD, a neurosurgeon with Mayfield Brain & Spine.
Because of the complexity of her condition, Dr. Kachmann in turn brought in a second spine specialist, Mayfield's Zachary Tempel, MD. The two surgeons have developed a team-based approach and perform complex reconstructive operations together every week.
Although complex reconstructions are not always performed with two surgeons, recent studies have shown that having two surgeons promotes efficiency while reducing time spent under anesthesia, hospitalization, complications, and blood loss. "It's always useful to have four experienced hands and two brains planning and analyzing the intraoperative events to carry out the operation effectively," Dr. Tempel says. "These operations are mentally and physically taxing, so two surgeons make for more efficient work."
Together, Drs. Kachmann and Tempel went through the exhaustive process of reviewing Lisa's x-rays, MRI scans, and myelogram. Like the reconstruction of a multi-story building, they measured, analyzed, and agreed on how each level of her spine would be addressed.
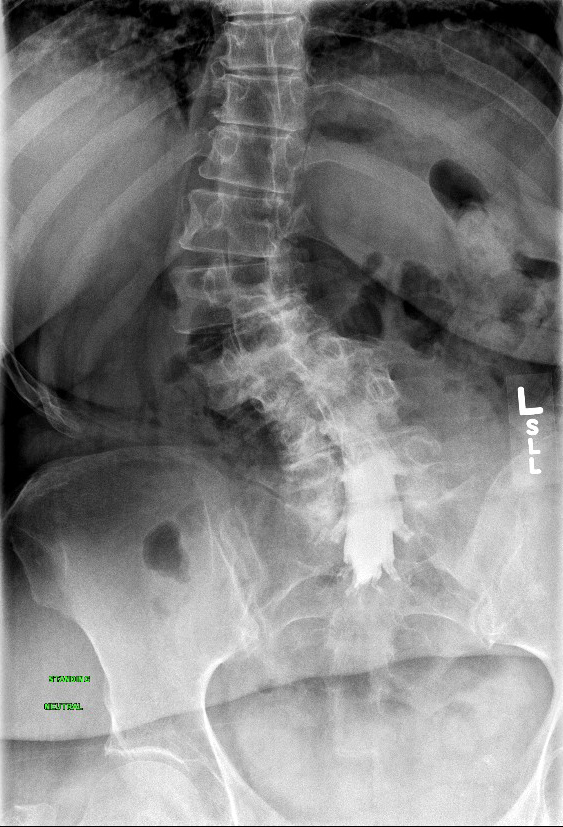
Lisa's spine before surgery

Lisa's spine post-op
In September 2018 Lisa underwent a two-part spinal deformity procedure at Good Samaritan Hospital. During Lisa's first surgery, Dr. Kachmann removed discs in her lower back, inserted cages into the disc space, straightened her spine, and restored a more normal curvature. An incision was made in her abdomen (by a vascular surgeon) – an anterior approach -- and in her side, a lateral approach.
"We stopped there, because doing the whole operation over 9 or 10 hours is too much," Dr. Kachmann says. "It also allowed Lisa to stand up after surgery and for us to get another x-ray of her spine. This is important because we had changed her spine a fair amount after the first day, and new images gave us a better understanding of what we had to do the second day."
Two days later, Drs. Kachmann and Tempel approached Lisa's spine from the back, a posterior approach. They performed osteotomies, the careful cutting of bone, and maneuvered her rotated spine into its best possible position. They anchored their work with rods that were secured in the vertebrae with pedicle screws.
"This is the kind of surgery that gets us out of bed in the morning," Dr. Tempel says. "It's the exciting stuff. It's also the stuff that keeps us up late at night. There are lots of unknowns, other factors that you can never predict with these kinds of operations, and we call a lot of audibles at the line of scrimmage because things can change on a dime."
For Lisa, the only hitch was her difficulty with anesthesia following the first operation. "I had a long night in recovery," she says. "I had a fantastic nurse that night, but I had a terrible reaction to some of the anesthesia. The next day I remember Dr. Kachmann saying, 'Tomorrow is going to be the big one,' and I thought, 'oh no, tomorrow is the big one?' Because yesterday felt like the big one. But they changed my medicine, and it was so much better the next day. I woke up and thought, 'The pain is gone.' I woke up a new person."

Lisa remained in the hospital for six days. She left the hospital in a brace and was advised to continuing wearing it for a total of 3 months whenever she used the stairs, went outside, or drove.
At a follow-up appointment 7 weeks later, the surgeons reviewed Lisa's new x-rays, declared her an "all-star," started her on physical therapy, and gave her permission to return to work 5 weeks later.
"I'm so thrilled with the outcome," Lisa says. "I'm so proud of myself for doing it. It's life-changing, physically, mentally, emotionally. I know where I am now, and I know where I was before surgery. I don't know where I would be in 10 years without surgery."
Lisa did observe that she had lost strength in her legs and was "still hobbling a bit." Not surprising, said Dr. Tempel. "This is part of the healing process, and often patients who undergo complex reconstruction have to retrain themselves to ambulate and rehabilitate back to doing normal activities."
Lisa's family and neighbors played an important role in her recovery by helping her with cooking, shopping, and other household chores. Her mother, Pat, a self-described "tough-love caregiver," made sure she didn't help too much, however. "Anything Lisa could do on her own, I wanted her to do on her own," Pat says.
Lisa's dog, a 14-year-old Cairn terrier mix, had to make his own adjustments. "He knows I'm slower, so he had to be slower," Lisa says. "When we go outside he doesn't pull on the leash anymore. He's been very good. We've had a lot of adjustment establishing who's in charge."
~ Cindy Starr
Hope Story Disclaimer -"Lisa's story" is about their health-care experience. Please bear in mind that because every patient is unique, individual patients may respond to treatment in different ways. Results are influenced by many factors and may vary from patient to patient.
